I have always wanted to visit Amsterdam. As a little girl I lived in Hershey, Pennsylvania, home of the Pennsylvania Dutch. Tulips have always been my favorite flower, and as a third grader, I wrote the embassy in Holland for a school project. Wooden shoes were neatly tucked alongside my gifts from Santa under the Christmas tree that year. I was smitten with the Dutch.
Who would have thought that it would be the stillbirth of my precious granddaughter Roberta Rae that would bring her grandparents to Amsterdam? The 2014 International Conference on Stillbirth, SIDS and Baby Survival, was held in Amsterdam this past September. My husband Mark and I had the privilege and honor of attending and representing Project Alive & Kicking (PAK). The conference was sponsored by the International Society for The Study and Preventions of Perinatal and Infant Death (ISPID) and the International Stillbirth Alliance (ISA).
There were 460 attendees, fifty of which were parents. We wondered why the number of parent attendees was not higher. Plenty of committed and dedicated researchers were present, but we thought there would be more obstetricians, maternal fetal specialists, midwives, doulas, nurses, pediatric neonatologists and all those who deliver care to our expectant moms and their babies.
SIDS
SIDS was a dominant topic throughout the conference.
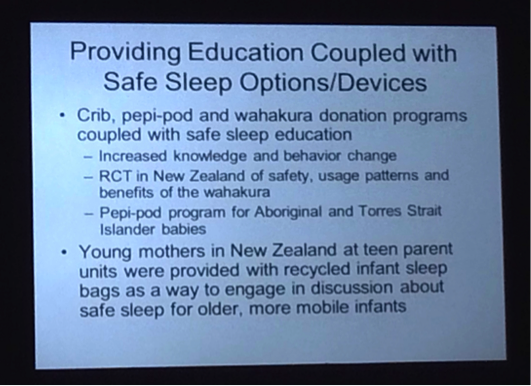
Dr. Rachael Moon from Baltimore, MD, spoke at length on creating “Safe Spaces” for babies, crucial for infant survival. She realizes that the frequent reminders of how to prevent SIDS are necessary for parents. So now texting, emailing and short videos relay the message of preventing SIDS.
The DOSE Program in Baltimore evolved through the astute observations of first responders answering daily 911 calls. As responders recurrently spotted infants at risk for SIDS in homes on unrelated calls, they knew something had to be done. Maybe a baby sleeping was on a sofa cushion, or on a family’s member’s chest in a recliner. Or a baby was covered with numerous blankets as a family member was smoking or drinking a beer nearby. These situations now turned into SIDS proactive home education visits with parents and family members by the first responders. Safe sleeping spaces for babies were created and the risk factors for SIDS within the home identified. SIDS numbers continue to lessen.
While on the subject of SIDS, Dr. Ed Mitchell from Australia gave a very informative lecture. Although many parents love to cuddle and sleep with their babies in their own bed, according to Mitchell, “Bed sharing is a risk for SIDS!” He stated that bed sharing is implicated in 90% of SIDS deaths.
Mitchell tells us that bed sharing and alcohol is a deadly combo but bed sharing, alcohol and smoking is a lethal combo and accounts for 2.8 SIDS deaths per 100. He stresses a “Safe Sleep Space” consists of a baby on his or her back, no smoking, no bedding and no alcohol.
Stillbirth
As Stillbirth is our passion, Mark and I were very impressed to learn that Professor Jason Gardosi from England is lowering the stillbirth rate in the UK with the implementation of the Growth Assessment Protocol (GAP) program. This method measures fundal height and suggests placental insufficiency to the health care team if the measurement is lower than the gestational week. Gardosi would like to see 4.5 ultrasounds from 32 – 40 weeks gestations to detect Intrauterine Growth Restriction (IUGR). With the impressive number of centers and hospitals using this program and the decrease in the stillbirth rate, parents now call the hospitals and centers they plan on using for prenatal care to see if Gardosi’s protocol is being used. Please visit projectaliveandkicking.org, My Pregnancy, Second Trimester, Week 21 to learn more on the importance of measuring fundal height and a link to Professor Gardosi’s work!
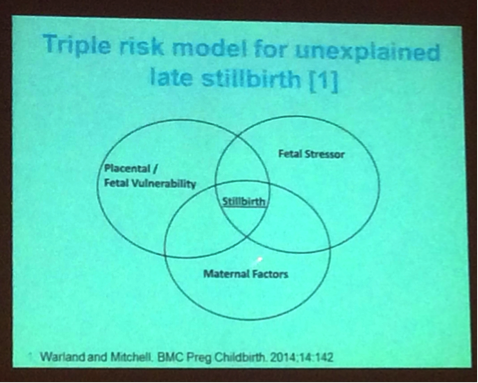
The placenta was the subject of discussion on several occasions. Dr. Jane Warland from Australia who is on PAK’s Medical Advisory Committee (MAC) shared with Mark and I the following slide below. She worked on the theory of Triple Risk Model for Unexplained Late Stillbirth with Dr. Mitchell. Both researchers agree that when a pregnancy has the elements contained in each of the three circles below present, placental/fetal vulnerability, fetal stressor, and maternal stressor, their central intersection point to the possibility of a stillbirth occurring. I call this “the perfect storm.”
Prior to this conference there were 62 classifications for the pathology of the placenta. Placental pathologists and researchers decided that it was time for one new placental model to be used by all. Of the 46 placental researchers invited to decide upon a new placental model, 26 met to make this amazing feat happen, and it did! There is now only one classification that will hopefully be used by all placental pathologists.
Mark and I met with Dr. Alex Heazell from Manchester, England. Heazell has received a substantial grant from the National Health Service (NHS) to improve the maternal and fetal outcomes of pregnancy. He shared is currently working on a blood test that could be ready for use by pregnant women in five years. This simple blood test would correlate with placental function, meaning that it would let the health care team know if the placenta is adequately functioning during pregnancy. Decreased fetal movements is another topic high on Dr. Heazell’s research agenda. He also stressed that the National Institute of Health (NIH) should be taking charge of stillbirth research and awareness in the US. He believes that the one way to get the NIH involved is to get PAK’s community involved in the foundation. It is only through the convergence of all those involved with stillbirth that a change could be implemented.
Next year will bring an update on the Lancet Series with Decreased Fetal Movements (DFM) being a major focus. In highlighting the Lancet Series from 2011, we were reminded of some key facts and findings. The figures used by The Lancet for stillbirths in this series were from 28 weeks gestation onwards. It was noted that “the data would not be as good” if the stillbirths figures were calculated from 20 weeks gestation as an additional 8 weeks gestation added to the stillbirth equations would make the figures much higher.
The Lancet Series also reviewed that stillbirth in labor “should not happen.” While the C-section rate in some countries is less than one percent, it is strongly felt that if the simple intervention of a C-section were to be increased, the stillbirth rate in tandem would drop. Globally, the two simple interventions that would help lower the stillbirth rates considerably are pregnant moms receiving folic acid and also being treated properly for malaria.
Dr. Ruth Fretts from Harvard spoke poignantly and tearfully on stillbirth citing it as a “tragedy and scandal.” Stillbirth is still the highest contributor to infant mortality at seventy percent. AIDS, various Congenital Malformations, and SIDS claim the remaining thirty percent of our babies.
She informs us that strikingly most stillbirths are not accounted for. With possibly thousands of “invisible” stillbirths occurring every year, the need for research is imperative. Soliciting funds is not easy for the stillbirth community, as the public does not understand the plight of the stillborn family. Fretts’s disappointment is obvious when she states, there is “no money in stillbirth” that is necessary for desperately needed research.
Insurance companies are not covering the simple stillbirth basics such as infant autopsies following delivery. Is this lack of insurance funding due to the fact that the OB community never mentions the possibility of stillbirth to moms during pregnancy? One OB from Indiana that we chatted with at the opening night party told us that she never mentions stillbirth because pregnancy is such a happy time. I asked her, “Well with 26,000 stillbirths occurring yearly, if you don’t tell moms who will?” Most moms are unaware that stillbirth still exists and the high numbers of babies it claims each year. Fretts shared a mom’s heartbreak when she questioned, “How come no one told me about stillbirth until we had one?”
The statistics of enduring a stillbirth in the USA is frightening; especially shocking is the statistics for black women.
White women – 1/202
Hispanic women – 1/183
Black women – 1/79
The current staggering number of stillbirths is incomprehensible and demands answers. Fretts told us of two programs that fight hard to diminish child and maternal mortality numbers. The first is called Child Survival. Having accrued thirty years of data, this program saves the lives of children under the age of 5 while promoting healthy and productive families and communities, The second, in existence for twenty years, is Safe Motherhood, which strives to implement the interventions that can reduce maternal mortality and morbidity. Yet, as we endure countless stillbirths that are not accounted for, there remains no world policy agenda or millennium goals on stillbirth according to Fretts.
One of our main concerns is why the American College of Obstetricians and Gynecologists (ACOG) has not adopted a protocol to be used universally in the US for expectant moms who experience Decreased Fetal Movements (DFM). A protocol is in place in various countries such as the UK and Australia. If you go to the ER or L&D with DFM in the USA, it is the doc of the day who will determine if you are thoroughly assessed or quickly discharged.
According to Fretts, the evolving stillbirth research encourages:
- Left side sleeping for all expectant moms.
- Diagnostic DNA microarrays testing that accurately diagnoses a genetic abnormality as the cause for fetal death. This provides closure for families, prevents unnecessary treatments, and enables clinicians to more accurately counsel and manage subsequent pregnancies.
- The improved evaluation of Decreased Fetal Movements (DFM) by both researchers and health care teams.
- The improved detection of abnormal growth in utero of both small for dates and large for dates babies.
- The optimal time of delivery based on mom’s gestational history.
Fretts does not support the newly adopted 39 Week Rule imposed by insurance companies, hospitals and health care teams meaning no baby will be delivered electively before 39 weeks unless there are extenuating circumstances. She tells us that the March of Dimes is praising the “new” ACOG guidelines on this induction of labor rule as this criteria helps fight preterm birth. Devastatingly, the stillbirth rate is increasing under the 39 Week Rule.
So as this conference to champion baby survival came to an end, Mark and I realized just how much work needs to be done to educate the public about stillbirth and the countless moms, dads, doctors, nurses, midwives, doulas and more that we have to reach. The latest research is telling us that we can save babies. Awareness, a proactive attitude and vigilance adopted by each expectant mom and her health care team will make a difference. PAK is playing a major role in making this feat happen.
But it’s the simple questions that Mark and I grapple with. We still need to know:
Do the obstetricians, midwives and those responsible for making sure that each and every mom delivers a healthy baby know that there are 26,000 stillbirths each and every year in the US?
Do they know that our stillbirth numbers are much higher than the 26,000 tallied every year in the USA?
Do they know? Do they really know?
The next Baby Survival Conference is in Buenos Aires, Argentina in 2016. We all have two years to learn Spanish and find out exactly where Argentina is on the map! Let’s all go to South America together and begin making the much needed difference. There is power in numbers. Let’s work alongside each other making stillbirth a globally recognized and accepted term, and vigorously diminish its numbers.


Connie,
Thank you for sharing your trip and informative blog post!! I can be your translator for next years trip to Argentina. 🙂
Donna
Oh thank you Donna. I would really appreciate you help for the conference in Argentina!